Rehab Case Study
Mr. S was admitted to Elmhurst Rehabilitation and Healthcare Center on July 20, 2022 under the care of Dr. Ali Akhtar. During the course of the stay, Occupational Therapy, Physical Therapy, and Speech Therapy were initiated to efficiently and effectively identify his unique needs and tailor specialized treatment plans to successfully transition to the next level of care.
On admission, he was noted to require maximal assistance with lower body dressing, moderate assistance with bathing and toileting and minimal assistance with hygiene tasks, upper body dressing, bed mobility, ambulation and transfers. Decreased balance and deconditioning also increased his risk for falling. He has been working with the interdisciplinary team and participating in care plan meetings and therapy throughout his stay. His participation was limited in the beginning of his stay due to weakness and overall deconditioning, but as he improved and increased his strength, he was able to increase his participation in higher level functional activities.
The therapy team provided skilled interventions to address his adaptation, compensation, and restoration potential and coordinated with the interdisciplinary team to ensure appropriate clinical care areas were addressed. On August 02, 2022, he successfully discharged home being able to complete bathing, hygiene tasks, dressing, toileting, bed mobility, ambulation and transfers independently. Great work Mr. S!
The rehabilitation length of stay was 14 days.
Case Study
Admitting Diagnosis: Muscle Wasting and Atrophy; Covid-19
Discharge Location: Home
Mr. C.A. is an 81-year-old male who was admitted to Elmhurst Rehabilitation and Healthcare Center from The Miriam Hospital for continued skilled nursing and rehab services for muscle wasting and atrophy. His stay was complicated when he was found to test positive for Covid-19. Upon admission, Mr. A. was evaluated by and participated in skilled occupational, physical and speech therapy where he was noted to require minimal to moderate assistance for most self-care tasks, contact guard assist for transfers and ambulate 20 feet with hand-held assistance and was noted to have recently been upgraded from a puree diet in the hospital and was being monitored to ensure safety was maintained during swallowing activities. He worked hard with his nursing and rehab team and as he progressed with therapy, he was able to participate in higher functional activities to ensure his safety was maintained. Upon discharge, Mr. A. was able to perform all self-care tasks with supervision, perform bed mobility with modified independence, transfer and ambulate up to 500 feet at a time with supervision, ascend and descend 3 stairs with supervision and was able to maintain his safety during swallowing activities on a mechanical soft diet. Great Work, Mr. A.!
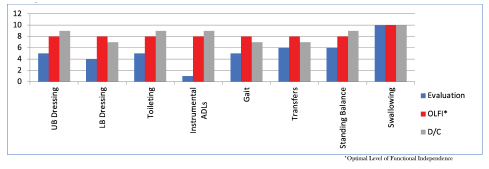
10.0 – Complete Independent – No assist, no equipment
9.0 – Modified Independent – No Assist, but equipment or extra time
8.0 – S/u – No physical assist other than set-up; supervision for safety/technique; and/or single cue to initiate
7.0 – Supervision-No physical assist; supervision for safety/technique; and/or single cue to initiate
6.0 – SBA-Pt. performs task with close supervision and or visual/verbal cues for task completion
5.0 – CGA – Contact Guard Assist
4.0 – Min – Occasional assist (25% or less time or effort to complete)
3.0 – Mod – Frequent assist (40-50% of the time or effort involved to complete task
2.0 – Max – Constant assist (75-90% of the time or effort involved to complete task
1.0 – CD – Complete Dependence: No contribution from pt; task done by others or not assessed
Case Study
Admitting Diagnosis: Parkinson’s Disease
Discharge Location: Home
A 65-year-old male was admitted to Elmhurst Rehabilitation and Healthcare Center from The Miriam Hospital with weakness, tremors, and a question of Parkinson’s disease to be addressed as an outpatient. Upon admission, Mr. S. was evaluated by and participated in skilled occupational and physical therapy where he was noted to require setup to contact guard assistance for most self-care tasks and supervision to transfer and ambulate 150 feet with a single point cane. He worked hard with his nursing and rehab team and participated in interdisciplinary rounds to assist in the achievement of his highest functional potential. Upon discharge, Mr. S. was able to perform most self-care tasks independently and was able to transfer, ambulate up to 500 feet at a time with a single point cane and ascend and descend 4 stairs with modified independence. Great Work, Mr. S.!
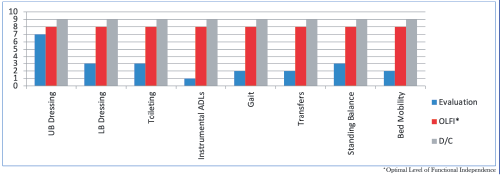
10.0 – Complete Independent – No assist, no equipment
9.0 – Modified Independent – No Assist, but equipment or extra time
8.0 – S/u – No physical assist other than set-up; supervision for safety/technique; and/or single cue to initiate
7.0 – Supervision-No physical assist; supervision for safety/technique; and/or single cue to initiate
6.0 – SBA-Pt. performs task with close supervision and or visual/verbal cues for task completion
5.0 – CGA – Contact Guard Assist
4.0 – Min – Occasional assist (25% or less time or effort to complete)
3.0 – Mod – Frequent assist (40-50% of the time or effort involved to complete task
2.0 – Max – Constant assist (75-90% of the time or effort involved to complete task
1.0 – CD – Complete Dependence: No contribution from pt; task done by others or not assessed






